As the global pandemic continues, plunging weight onto all kinds of people in all kinds of situations, social media abounds with shocking statistics, escapist humor, and toxic misinformation.
Some on the front lines, though, are using the platforms to share their stories and humanize the far-away numbers of a crisis.
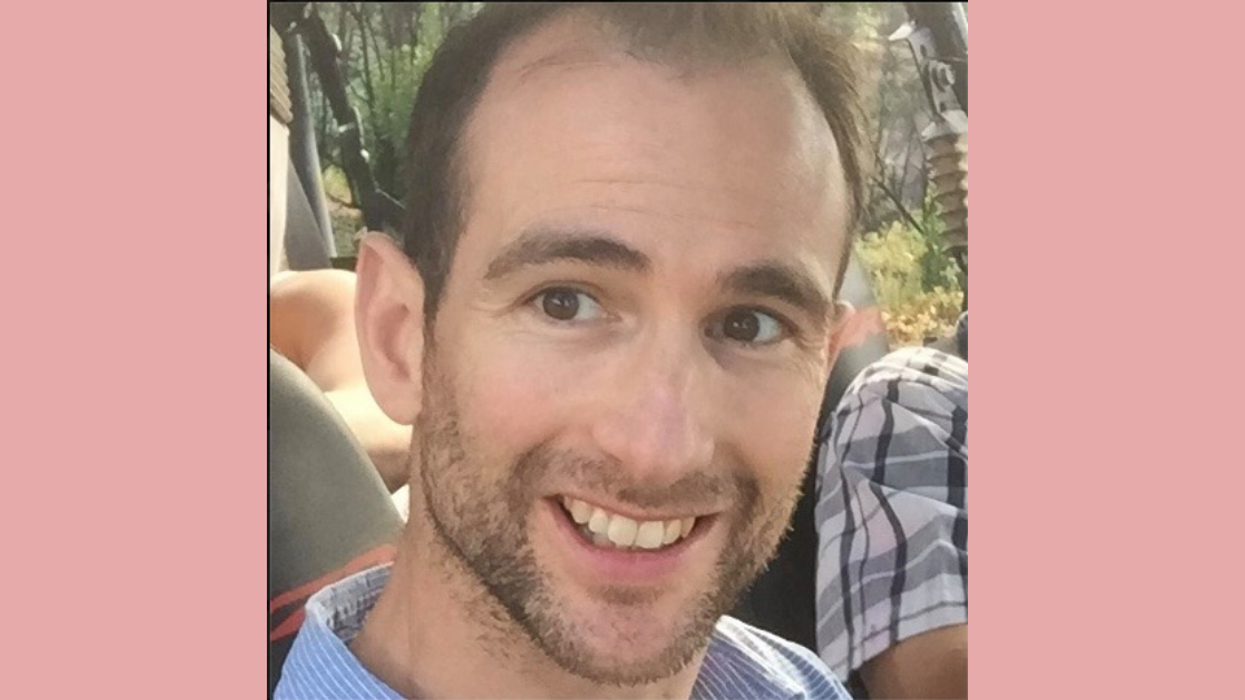
Nick Dennison is a consultant anaesthetist at Frimley Park Hospital, just south of London.
He typically spends his days carrying out the very specific duties of his specialized role in the medical community: managing pain and patient awareness throughout surgery using the ideal drugs.
But Dennison's concentration to those isolated job functions have not remained in tact while the virus overwhelms the hospitals of Britain, as it has the hospitals all around the world. He, like many colleagues, have been forced to become intensive care doctors overnight.
And for Dennison, that change does not occur in a vacuum, as a lengthy Facebook post elaborated.
"My son turned three years old last week and is six weeks into a three year chemotherapy program for lymphoma. This virus is a big threat to his life and as I am going to be exposed this week doing my job, I can no longer live at home."
"I have had to make the difficult choice: to do my job and save lives of people I don't know, or to be with my son whilst he battles cancer."
"Alfie hopefully will survive his cancer and chemo, but many people will die from flu. My heart is broken making this decision, but I choose to save the lives of strangers and leave him in the care of my beautiful wife and family."
Comments to the post were wildly supportive of the sacrifice.
In addition to that heartbreaking description of sacrifice, Dennison's post also served to offer more objective information. He clearly outline what is happening in hospitals due to the overwhelming increased demand.
"I'm a consultant anaesthetist working in Frimley Park Hospital and this week all anaesthetists are being re-roled as intensive care doctors. We will be tasked with putting the sickest patients under anaesthetic and onto ventilators/life support machines."
He quickly addressed the elephant in the room: the well-known fact that, nearly everywhere, there are more patients than ventilators.
"Each patient will require 10 days+ on a ventilator then may need a temporary tracheostomy to get them off the ventilator."
The Mayo Clinic defines a tracheostomy as, "a hole that surgeons make through the front of the neck and into the windpipe (trachea). A tracheostomy tube is placed into the hole to keep it open for breathing."
Dennison did not hold back as he outlined the top heavy numbers and dire medical inadequacy.
"The intensive care unit is already full of COVID-19 patients on ventilators (12) with more requiring ventilation every day. My hospital usually has 4-10 patients on ventilators and is planning and EXPECTING 80 patients to require ventilation."
"It seems the public health message is not getting through. Let me be clear. A lot of people are going to die. They will mainly be 70 years plus but be in no doubt, 30-40 year olds will die too."
The doctor then shifts his tone, using his platform to urge pre-emptive behavior change.
"Pubs have been busy, offices open, social events happening, kids parties etc. It all needs to stop. Infected people shed virus and it must be everywhere by now. It is your social responsibility to engage in social distancing."
"Actions NOW can prevent further disease transmission, ICU admissions and deaths in 10-20 days."
Many comments illustrated that the doctor's words galvanized some urgency around social distancing.
Near constant and repeated messages advocating social distancing as a key mechanism to slow the spread of the virus have been made for weeks. It becomes clear that only when those are taken very seriously will those experts be given the chance to catch up to the work.











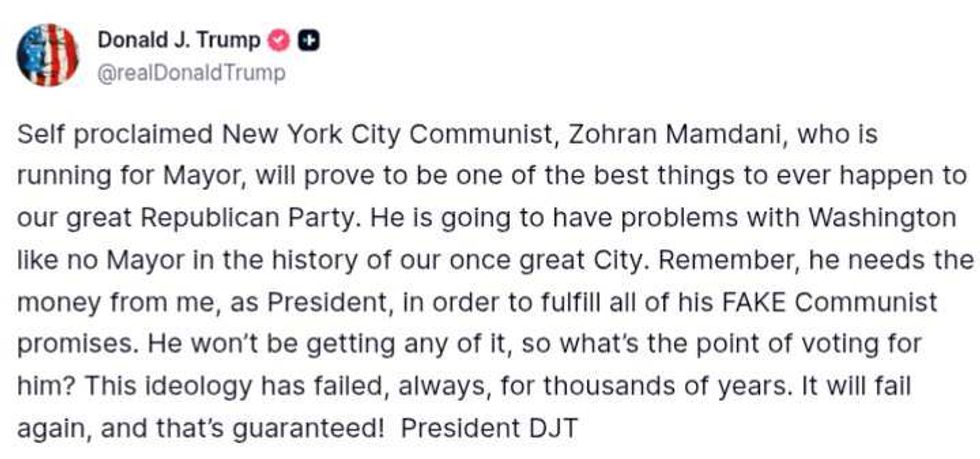 @realDonaldTrump/Truth Social
@realDonaldTrump/Truth Social

 Who Does That Sutton Foster GIF by YoungerTV
Who Does That Sutton Foster GIF by YoungerTV  garlic cooking GIF
garlic cooking GIF  Red Hair Wow GIF by CompanyCam
Red Hair Wow GIF by CompanyCam  Lightning Thunder GIF by Tec de Monterrey
Lightning Thunder GIF by Tec de Monterrey