In February, a 30-year-old woman in New York City became the first male-to-female transgender person to breastfeed a baby.
When the transgender woman told doctors at the Mount Sinai Center for Transgender Medicine and Surgery in New York that she wanted to breastfeed her pregnant partner’s baby, they put her on a regimen of drugs that included an anti-nausea medication licensed for use in Britain and Canada but banned in the United States.
Within a month, she was producing droplets of milk. And within three months — two weeks before the baby’s due date — she had increased her production to eight ounces of milk a day.
Ultimately, after undergoing a three-and-a-half month experimental treatment regimen, she was able to rely exclusively on her breast milk for the baby’s first six weeks. At week six, she was still producing a maximum of 227 grams per day. This number represents about half of the number of grams of milk that a newborn requires daily after five days of age, but the baby developed normally and in good health. After six weeks, the mom supplemented with formula.
How Did She Do This?
The couple worked with Dr. Tamar Reisman and Zil Goldstein, a nurse practitioner, at the Mount Sinai Center for Transgender Medicine and Surgery in New York City.
As reported in Volume 3.1, 2018 of Transgender Health, “the patient’s medical history was significant for gender incongruence for which she initiated a feminizing hormone regimen in 2011. At the time of our first visit, she was taking spironolactone 50 mg po bid, estradiol 2 mg po bid, and micronized progesterone 100 mg po bid.”
In essence, the recipe for this mother’s milk was years in the making. Long before her partner became pregnant, she had been taking female-enhancing hormones. At five-and-a-half months through the pregnancy, a combination of breast stimulation, oral hormones and nausea medication was introduced. Prolactin, the hormone produced organically in breastfeeding women, is not available as a lab-made alternative. Instead, the new mother used an anti-nausea drug called Domperidone as a prolactin replacement. Along with the Domperidone, she used three hormones: estrogen, progesterone and spironolactone (this last hormone blocks the production of testosterone).
At the woman’s one-month follow-up doctor visit, she was able to produce just a few droplets of milk. But at her three-month follow-up visit, just two weeks before the baby’s due date, she was able to produce eight ounces.
The report in Transgender Health continues: “Three-and-a-half months after she had started the mentioned regimen, the baby was born weighing 6 lbs., 13 oz. The patient breastfed exclusively for 6 weeks. During that time the child’s pediatrician reported that the child’s growth, feeding, and bowel habits were developmentally appropriate. At 6 weeks, the patient began supplementing breastfeedings with 4–8 oz of Similac brand formula daily due to concerns about insufficient milk volume.”
Is This Safe?
Domperidone is an anti-nausea medication that is often used to combat morning sickness and vomiting during pregnancy. Like many medications, Domperidone has side effects. In this case, one side effect of this anti-nausea medication happens to be a beneficial one for the mother: increased lactation. It is for this reason that the transgender patient decided to use Domperidone, though not the purpose for which the drug was manufactured.
The U.S. Food and Drug Administration (FDA), however, warns against using Domperidone strictly for milk production, even for biological women who suffer from low or inadequate supply. While Domperidone is widely available throughout Europe for gastric purposes, it’s important to note that it is NOT approved in the United States nor any country for the sole purpose of increasing lactation. The published FDA report states: “There have been several published reports and case studies of cardiac arrhythmias, cardiac arrest, and sudden death in patients receiving an intravenous form of domperidone that has been withdrawn from marketing in a number of countries.”
The study also states that there is no long-term research on how children are affected by the use of Domperidone during infancy. But, when tested on laboratory animals, high doses of domperidone over an extended period resulted in breast tumors. Discontinuing the use of the product must be done over a period of weeks, slowly decreasing both the dosage and frequency. In a cisgender woman, this slow weaning process is intended to help the mother’s body continue to produce the same amount of milk. Without the domperidone, the transgender woman cannot produce milk on her own.
Spironolactone is one of a class of drugs known as diuretics, which help expel water and salt and have been traditionally used to treat high blood pressure. Medical professionals seem to be in agreement that the use of Spironolactone is acceptable during pregnancy and breastfeeding when the mother has high blood pressure, glaucoma or edema. Once metabolized, Spironolactone breaks down into a product called milk canrenone. A breastfeeding study showed that only two percent of the metabolite passed from the mother to the infant — not enough to suggest that the drug could harm nursing infants.
Progesterone and estrogen are hormones that are naturally produced in a female’s body. When these hormones are administered to enhance gender identity there are a few risks, which can include gallstones, high blood pressure, elevated liver enzymes, weight gain and cardiovascular disease.
The simple answer to the question “is it safe?” is yet to be determined. The infant would need to be tested and evaluated in the future for characteristics such as health of the immune system and overall IQ. Since there has not been, to date, adequate testing of the transgender breast milk, it’s impossible to know how, chemically, this woman’s breast milk compares on a molecular level to the breast milk of a cisgender female.
“This is a very big deal,” says Joshua Safer of Boston Medical Center, “Many transgender women are looking to have as many of the experiences of non-transgender women as they can, so I can see this will be extremely popular.”
But perhaps more importantly, there are tangible physical benefits for the newborn. As noted in Transgender Health: “Breastfeeding offers immunological, metabolic, and psychosocial benefits for both mother and infant. Breast milk contains secretory IgA, anti-inflammatory agents, and other immunomodulators that give breastfed infants immunological advantages relative to formula-fed infants. Formula-fed infants are noted to have higher risk of rotavirus infection, otitis media, hospitalization for lower respiratory tract infections, sudden infant death syndrome, necrotizing enterocolitis, asthma, and childhood obesity relative to their breastfed counterparts.
“In addition, breastfeeding offers economic advantages by allowing families to save resources that might be devoted to formula and infant healthcare.
Women who breastfeed are noted to have lower rates of breast cancer and ovarian cancer than women who have never breastfed. Breastfeeding has been noted to facilitate mother–child bonding.”
While not every mother may choose to breastfeed, those who want to should be able to, regardless of their sex at birth.








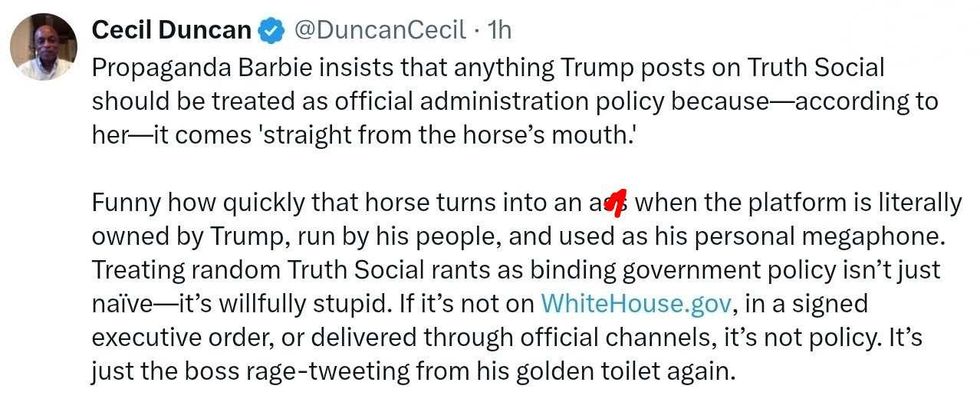 @DuncanCecil/X
@DuncanCecil/X @@realDonaldTrump/Truth Social
@@realDonaldTrump/Truth Social @89toothdoc/X
@89toothdoc/X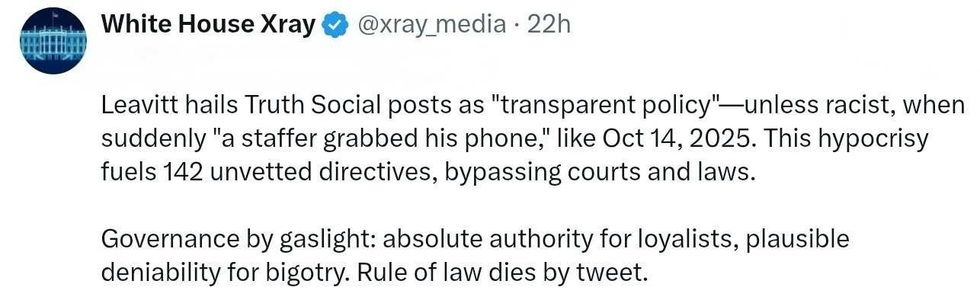 @xray_media/X
@xray_media/X @CHRISTI12512382/X
@CHRISTI12512382/X
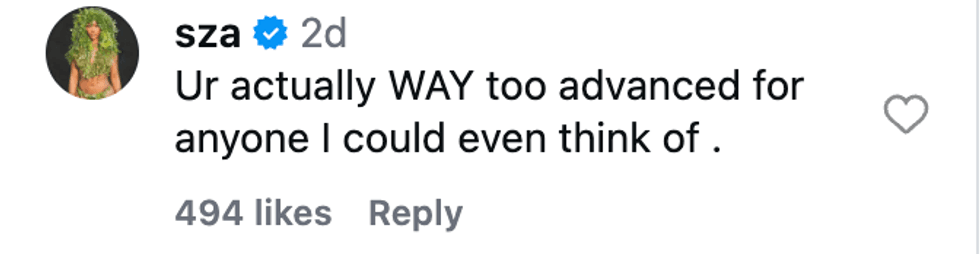 @sza/Instagram
@sza/Instagram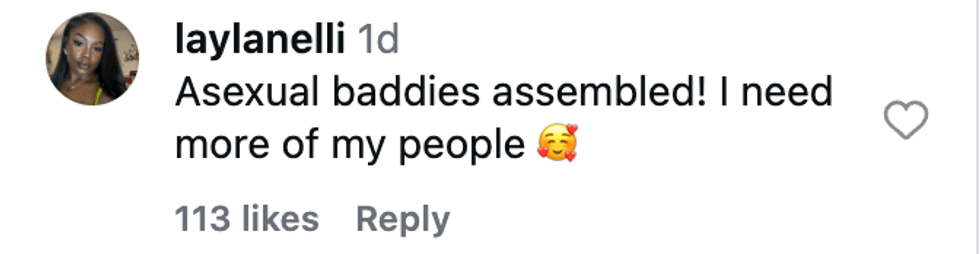 @laylanelli/Instagram
@laylanelli/Instagram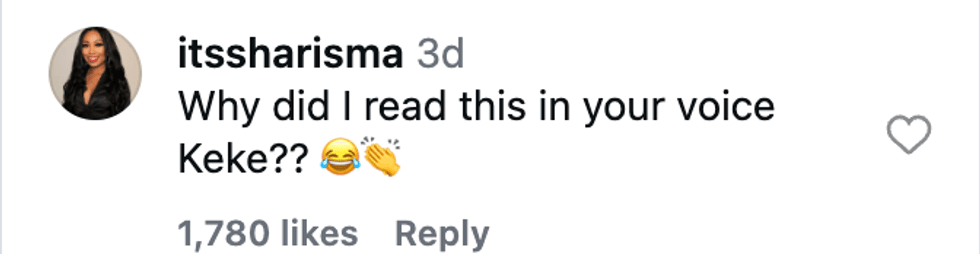 @itssharisma/Instagram
@itssharisma/Instagram @k8ydid99/Instagram
@k8ydid99/Instagram @8thhousepath/Instagram
@8thhousepath/Instagram @solflwers/Instagram
@solflwers/Instagram @msrosemarienyc/Instagram
@msrosemarienyc/Instagram @afropuff1/Instagram
@afropuff1/Instagram @jamelahjaye/Instagram
@jamelahjaye/Instagram @razmatazmazzz/Instagram
@razmatazmazzz/Instagram @sinead_catherine_/Instagram
@sinead_catherine_/Instagram @popscxii/Instagram
@popscxii/Instagram