Historically speaking, a woman’s value resided in the sum of her parts, her womb, her ovaries, the width of her hips, her sex, and her ability to give pleasure. This may be one explanation for why studies into women's health trail decades behind men.
If I were to ask you to list five signs of a heart attack, what would you come up with? If you said cold sweats or nausea, chest pressure or pain, shortness of breath, pain in one or both arms, chest, back or stomach pains, congratulations, the 50 years of research into heart disease has paid off. You correctly identified signs that can help save your father, son, brother, uncle or nephew from a heart attack.
But what about your mother, daughters, sister, aunt or niece? Despite the health education classes, emergency response training and the Public Service Announcements you grew up with, scientists have only begun studying heart disease in women in earnest over the last 18 years. So it has only been since then that we learned that the symptoms for a heart attack in women include lightheadedness or dizziness, upper back pain, fainting or fatigue, in addition to shortness of breath and chest pains, two symptoms shared between the sexes.
Between 1949 and 1999, the cardiovascular disease (CVD) mortality rate for men dropped precipitously as a result of the many studies performed during that period and the subsequent treatments that were developed. By 1999, CVD deaths in men dropped by 59 percent. However, cardiovascular disease in women rose and the mortality rate surpassed that of the mid-20th century numbers that spurred research into CVD in the first place. Until the early 2000s, 85 percent of participants in CVD studies were men. In 1990, the U.S. General Accounting Office (GAO) issued a report that showed that women with childbearing potential were systematically excluded from all phases of drug trials related to CVD. Women were even excluded when selections were supposed to be random, along with men 80 to 85 of age.
The report sparked a congressional investigation and propelled women's advocacy groups into action. In response to the pressure, the National Institute of Health (NIH) formed The Office of Research on Women’s Health. However, it was not until The NIH Revitalization Act of 1993 required, by law, that NIH-funded studies include women, that the Office of Research on Women’s Health became a funded federal agency. It is noteworthy that the office's initial creation was solely symbolical; it was not until the passing of the 1993 act did the agency have teeth and the funding to carry out its mandate.
The federal changes suggested an equal amount of dollars would be committed to women’s health research, and that, specifically, funds would be devoted to research into CVD, the number one killer of women in America. However, a 2013 report from the American Heart Association shows a commitment of $5,589,841 to the study of heart disease in women. This number topped the list of dollars committed to specific minority groups; Asian studies received the least with $52,000 being committed. However, stacked next to the $3.5 billion spent on research into CVD in the first 50 years of research, that number is dismal.
If a woman’s value is more than the sum of her parts, her womb, her ovaries, her hips, then her body as a whole should be protected. The key to providing this protection lies in equivalent and gender-appropriate research and education in women’s health. 1 in every 4 or 289,758 women died from a heart attack in 2013. If we saw the same 59 percent reduction men saw as a result of fifty years of research, 170,957 women’s lives would be saved.
It has been 25 years since the passing of The NIH Revitalization Act of 1993. We are not well on our way to dropping the mortality rate for women. Women’s heart attacks are still more likely to be misdiagnosed and most medical schools still do not incorporate what little we have learned about CVD in women in their classes. In 2018, why are the dollars committed to the study of CVD in women stagnant and the death toll still so high? If a woman received the same time, care, and adequate dollars as her male counterpart, we would be armed with the skills and tools to not only save our fathers, sons, brothers, uncles or nephews, but our mothers, daughters, sisters, aunts or nieces too. The question that begs to be asked, two and half decades into what should have been a period marked by advancements in the study of CVD in women, is both simplistic and damning:
What is the value of your mother’s, daughters’, sisters’, aunts’ or nieces’ life? Are they not worth saving too? The rhetoric says they are. However, actions and money say otherwise.









 @RichardLaub4/X
@RichardLaub4/X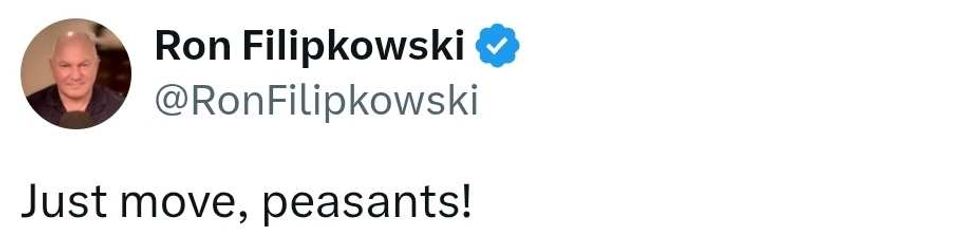 @RonFilipkowski/X
@RonFilipkowski/X
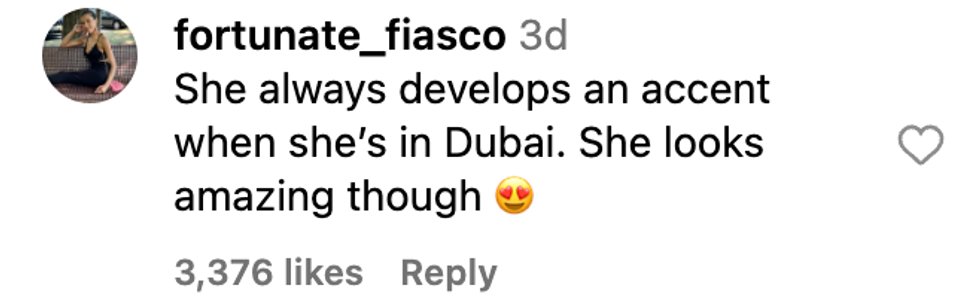 @fortunate_fiasco/Instagram
@fortunate_fiasco/Instagram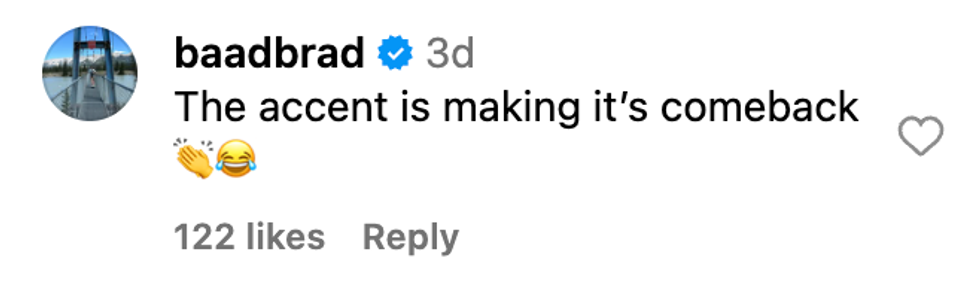 @baadbrad/Instagram
@baadbrad/Instagram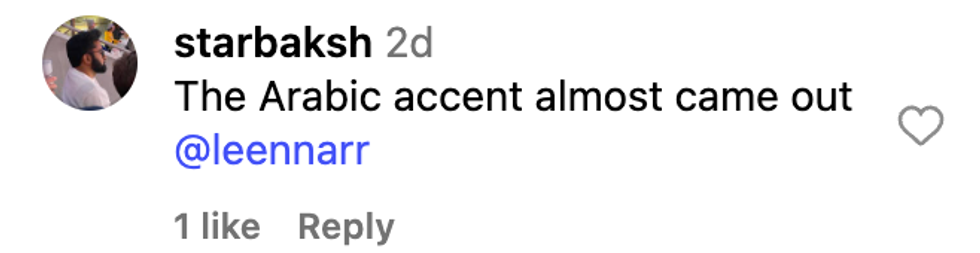 @starbaksh/Instagram
@starbaksh/Instagram @angelcartel/Instagram
@angelcartel/Instagram @tamoderos/Instagram
@tamoderos/Instagram @rinabekiri/Instagram
@rinabekiri/Instagram @grace.s.hamilton/Instagram
@grace.s.hamilton/Instagram @robbietomkins/Instagram
@robbietomkins/Instagram @mereyahncage/Instagram
@mereyahncage/Instagram @aristochick/Instagram
@aristochick/Instagram @rrmrrmrrmrrmrrm/Instagram
@rrmrrmrrmrrmrrm/Instagram @drewguy88/Instagram
@drewguy88/Instagram @annacollins5172024/Instagram
@annacollins5172024/Instagram @lvndrbeauty/Instagram
@lvndrbeauty/Instagram @dinalohan/Instagram
@dinalohan/Instagram
 @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok @jameelajamil/TikTok
@jameelajamil/TikTok