Immunotherapy represents a whole new approach for combating several types of human cancers. The tactic involves scientists genetically reprogramming the cells of a person’s immune system to target and attack malignancies. Immunotherapy is now considered the “fifth pillar” of cancer treatments, rapidly evolving into a more promising tool for battling cancer than standard radiation and chemotherapeutic treatments.
Although there are many different immunotherapies in development and practice, chimeric antigen receptor T-cells (CAR-T) therapy has shown the most promise to date. Indeed, CAR-T therapy is the first anti-cancer gene therapy to be approved by the United States Food and Drug Administration (FDA) for use against advanced adult lymphomas and childhood acute lymphoblastic leukemia. Unfortunately, just recently, a patient given CAR-T therapy for aggressive leukemia died as result of the treatment.
CAR-T is just one of multiple immunotherapies that are classified as “adoptive cell transfers” (or ACTs). ACT involves the collection of an individual’s immune cells which are then genetically reprogrammed in the laboratory via the introduction of specialized DNA constructs. T-cells are often the cell type selected for collection and genetic modification as they are one arm of the human adaptive immune response, which recognizes and devises an effective countermeasure to invading disease-causing agents. The DNA constructs introduced in the laboratory setting drive the expression of chimeric antigen receptors (CARs) in the T-cells that are displayed on the cell surface, which redirects them to attack cells that display markers common to certain types of cancers.
Dr. Carl June of the University of Pennsylvania Abramson Cancer Center has led several clinical trials of the CAR-T therapy and said that the receptors produced by this treatment are “synthetic molecules” that “don’t exist naturally.”
Most often, the incorporation and expression of the DNA constructs is accomplished using virus vectors that have been adapted to efficiently deliver genetic material. Using virus vectors in this way has been applied to the development of various forms of gene therapy as well as certain vaccine platforms. Depending on which virus has been chosen for the application, certain hurdles must be surmounted. For example, the virus used to deliver the genetic instructions may be recognized by the patient’s immune system, culminating in the genetic delivery vehicle being targeted. Also, there are safety issues that arise out of fear that the viral introduction of DNA might accidentally damage part of the host genome potentially leading to other health problems.
Most often the CAR genetic material is targeted to a molecule called CD19 that can be found on the surface of B-cells. B-cells are the antibody-producing arm of the human adaptive immune system and cancer development can sometimes lead to higher than normal expression levels of this surface protein. This unique marker on the surface of B-cells has been utilized as a means to specifically target B-cell driven lymphoma, chronic lymphocytic leukemia, and acute lymphoblastic leukemia. In the case of the CAR-T therapy, the reprogrammed T-cells seek out and attack the malignant B-cells displaying CD19.
CAR-T therapy has been referred to as a “living drug” since the patient is being treated with live cells, a person’s own T-cells. In the recent CAR-T related death, one of the patient’s cancerous B-cells was accidentally isolated along with the population of T-cells. This leukemic cell received the same genetic reprogramming that was given to the T-cells, which led to this single cell masking its CD19 receptor with the synthetic CAR. This allowed the cancer cell to hide from the CD19 targeted T-cells and to proliferate into a more aggressive cancer.
As described by Dr. Marco Ruella, whose team determined the cause of the CAR-T patient’s death: “If you have the CAR and you have the target in the same place, they bind each other. The CAR-T cells cannot see that CD19. This is an exceptionally rare event.” Dr. Ruella further commented that sometimes leukemic cells do make it into the batch of T-cells being re-programmed, but those cells almost always die off.
Since its development, the CAR-T therapy has been given to hundreds of patients, whether by one of the licensed treatments or during a clinical trial. Throughout these clinical studies, resistance has been observed to occasionally occur through mutations in the CD19 target.
Novartis, the manufacturer of Kymriah, one of the CAR-T therapeutics, asserted that its manufacturing process takes extra steps to prevent leukemic cells from contaminating the CAR-T cells. Gilead Sciences, the pharmaceutical company that produces the other licensed CAR-T therapeutic called Yescarta, has yet to comment on the recent CAR-T related death.
There have been other deaths associated with CAR-T based therapeutics in the past. In 2017, a patient died from a CAR-T treatment aimed at combating non-Hodgkin’s lymphoma that was produced by Kite Pharma. And the year prior, five deaths were reported from a now-suspended CAR-T clinical trial initiated by Juno Therapeutics. While it is still hailed as a breakthrough approach to beating back cancer, there have been fatal setbacks along the way to FDA licensure.
Alternative approaches to the production of the CAR-T therapeutic are being explored. For instance, a recent press release described a “non-viral, plasmid-free” CAR-T manufacturing method being investigated by two partnered companies called LineaRx, Inc. and iCell Gene Therapeutics, Inc. This new approach to the design and manufacture of the DNA constructs for CAR-T would make it less costly and less time-consuming. Also, the large-scale DNA production method touted by LineaRx, Inc. would eliminate the need for viral vectors that give some scientist and clinicians concern over potential recombination events in a person’s genome.
This recent tragic death has not deterred the pharmaceutical industry from its belief that CAR-T is a winning therapy and expansion plans are already underway. Indeed, capacity is being doubled for the production of the viral vector that is used by Novartis to deliver Kymriah into harvested T-cells. The platform called LentiVector is produced by Oxford BioMedica, who just locked in a lease for a manufacturing facility in Oxford, UK, that will double its existing capacity. Moreover, the LentiVector platform has been described to have overcome the safety and delivery issues problematic in earlier versions of the technology. Oxford BioMedica teamed up with Novartis in mid-2017 and is expected to receive $100 million from the partnership.






 @realDonaldTrump/Truth Social
@realDonaldTrump/Truth Social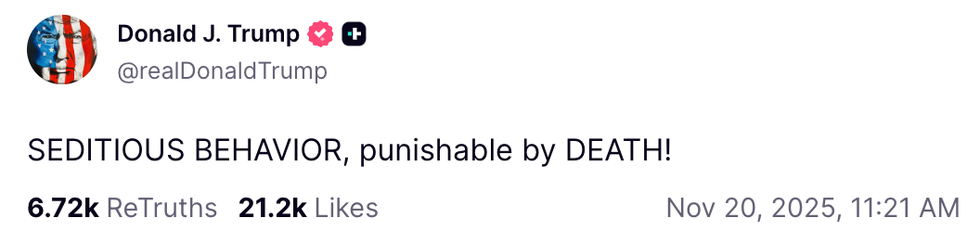 @realDonaldTrump/Truth Social
@realDonaldTrump/Truth Social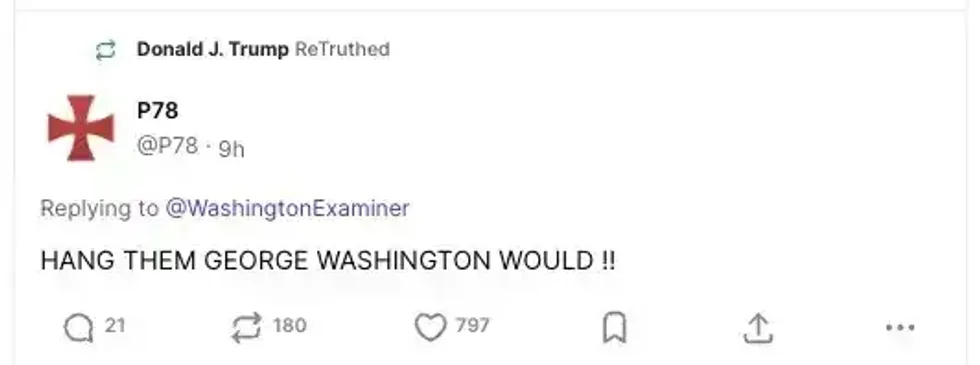 @P78/Truth Social
@P78/Truth Social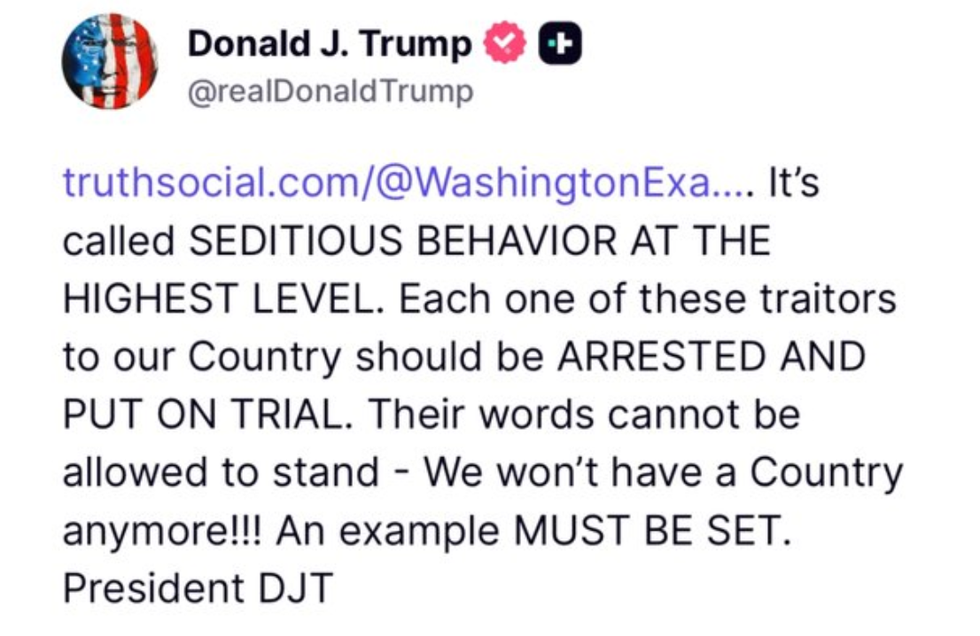




 big brother pop GIF by Big Brother After Dark
big brother pop GIF by Big Brother After Dark 
 Unimpressed Get It Together GIF
Unimpressed Get It Together GIF  The Bachelor Shut Up GIF by BuzzFeed
The Bachelor Shut Up GIF by BuzzFeed  customer service waiter GIF
customer service waiter GIF 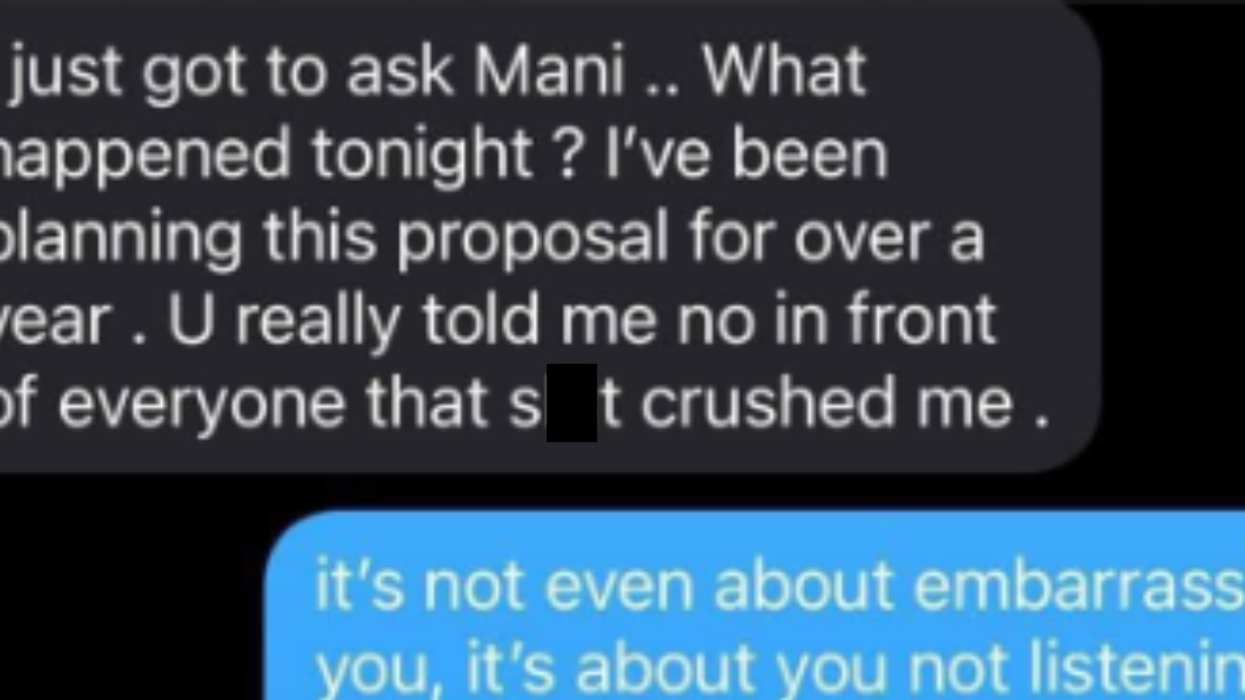
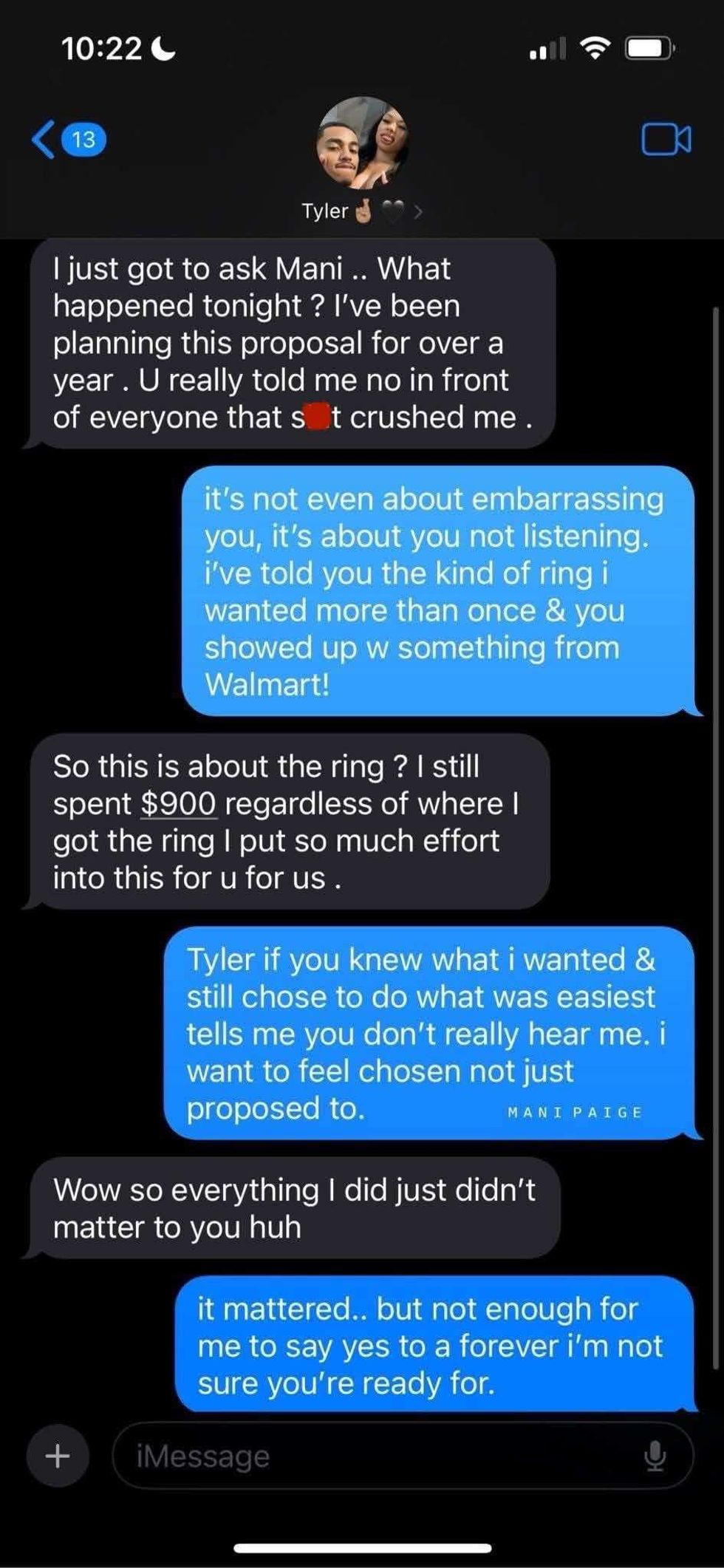 @prissyxoxo25/Threads
@prissyxoxo25/Threads @prissyxoxo25/Threads
@prissyxoxo25/Threads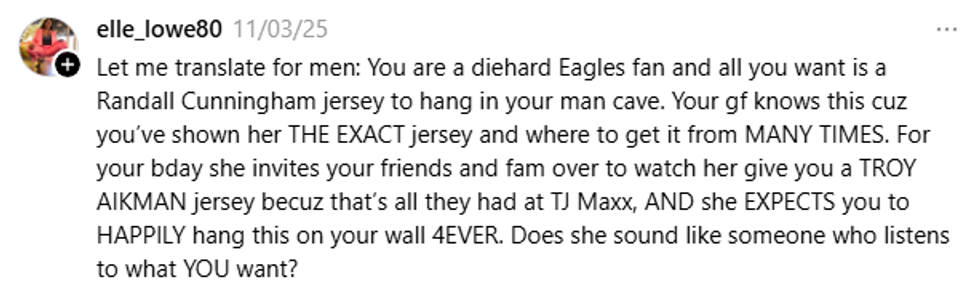 @prissyxoxo25/Threads
@prissyxoxo25/Threads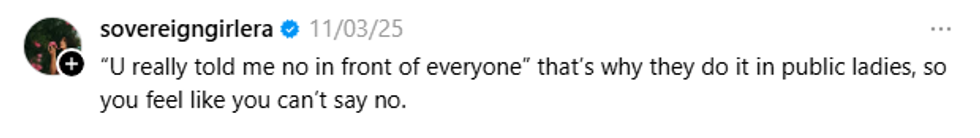 @prissyxoxo25/Threads
@prissyxoxo25/Threads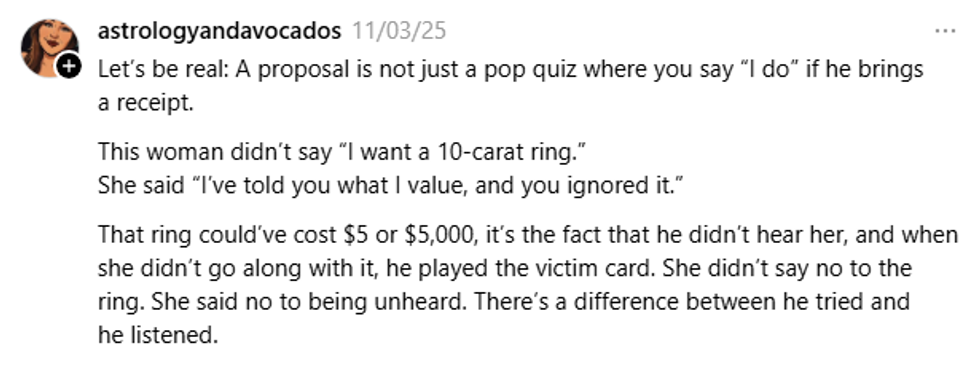 @prissyxoxo25/Threads
@prissyxoxo25/Threads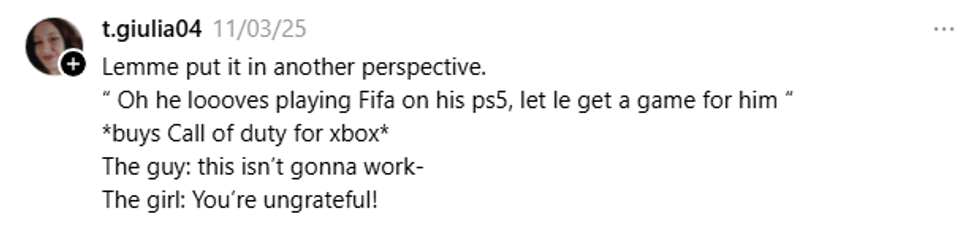 @prissyxoxo25/Threads
@prissyxoxo25/Threads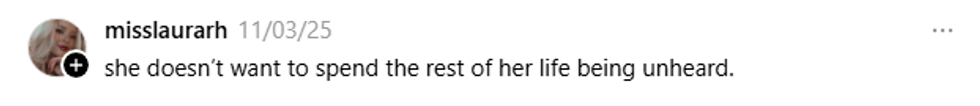 @prissyxoxo25/Threads
@prissyxoxo25/Threads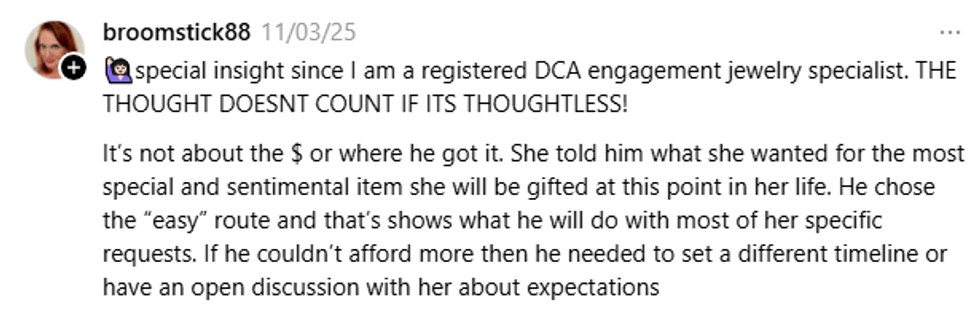 @prissyxoxo25/Threads
@prissyxoxo25/Threads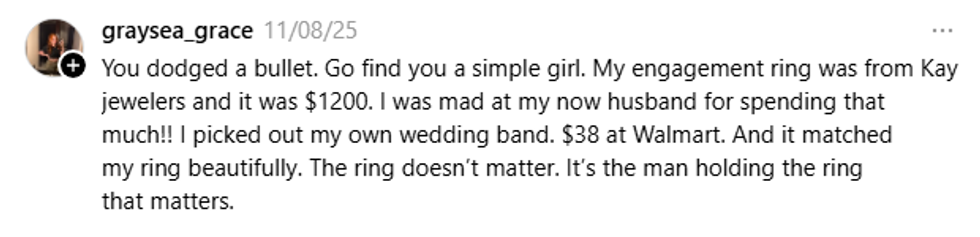 @prissyxoxo25/Threads
@prissyxoxo25/Threads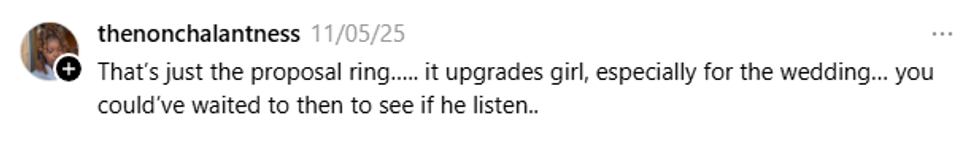 @prissyxoxo25/Threads
@prissyxoxo25/Threads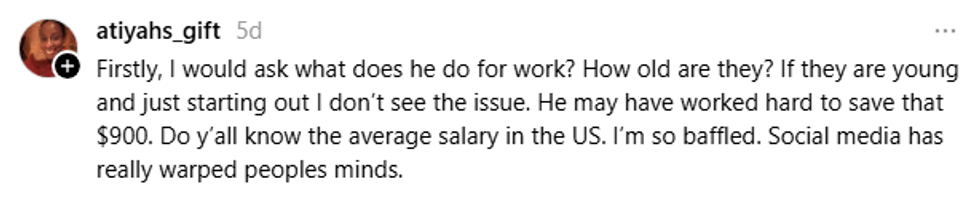 @prissyxoxo25/Threads
@prissyxoxo25/Threads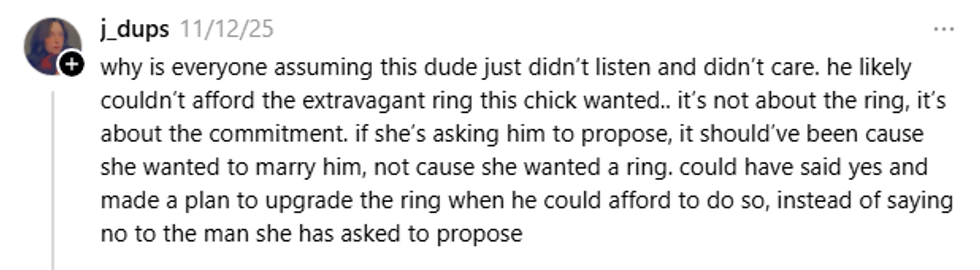 @prissyxoxo25/Threads
@prissyxoxo25/Threads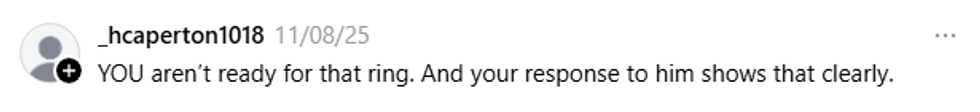 @prissyxoxo25/Threads
@prissyxoxo25/Threads
 @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok @randomthoughts2226/TikTok
@randomthoughts2226/TikTok
 @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok @lookitskateeee/TikTok
@lookitskateeee/TikTok