When a teenager in Idaho contracted the bubonic plague in early June, it made a few headlines because it was the first case in Idaho in 26 years. Half a millennium after it killed an estimated 60% of the European population, the specter of the Black Death still looms large in Western consciousness — gangrene, swollen lymph nodes, seizures — a horrific relic of days long past. But actually, although the bubonic plague has long been understood, it has never been eradicated.
In fact, outbreaks of the bubonic plague have been fairly common across the US since the early 20th Century. The last widespread outbreak happened in Los Angeles in late 1924, when 30 people who lived within a few blocks of each other contracted the bubonic plague, which developed into pneumonic plague, as it virtually always does when left untreated. Altogether, 24 people died in that outbreak, though newspapers at the time referred to it as a strain of pneumonia to prevent panic — and possibly anti-racist sentiment as the neighborhood affected was home to a large population of Mexican immigrants, including Patient 0. Antibiotics, which are still very effective against the bubonic plague, did not come into widespread use until the 1950s. Before that development, outbreaks were not unusual throughout the west, particularly in California, New Mexico, Arizona and Oregon.
The infection spread in those outbreaks exactly as it did in the Middle Ages, and as it did to the recent Idahoan victim: via fleas who infect rodents. In medieval Europe, the culprits were rats. In the modern United States, they’re fluffy rats. That’s right, ground squirrels (a group that includes chipmunks) are the suspected vector in the Idaho case. They’ve been known as carriers as far back as 1924, and Los Angeles health officials credit their rodent eradication program as the key to limiting that outbreak’s infections. As part of that effort, virtually all of the city’s ground squirrels were exterminated.
Rodents spread the disease via fleas carrying the Yersinia pestis bacteria, and rodents carrying that bacteria have been found all over the Western US, particularly in the Four Corners region. At least one case of the disease is reported there every year, and some years more than 10 cases have been recorded.
Around the world, though, bubonic plague remains even more common. Madagascar is particularly affected, with dozens of cases annually. During a 2017 outbreak there, officials asked native Malagasy to halt their sacred funerary rite, Famadihana, due to worries that the tradition of exhumation and ancestor worship may be causing new infections.
One reason that the plague is so widespread in Madagascar is that the disease’s early symptoms closely resemble malaria’s early symptoms, which is also endemic, and not nearly as contagious between humans as the bubonic plague is. The 2017 outbreak ultimately infected 2,348 and killed 202 people.
That outbreak survival ratio is fairly standard with modern antibiotic treatments: 90% of treated patients recover. Left untreated, however, the death rate still reaches the medieval levels of 30-90%.
The teenaged victim in Idaho, whose identity has been protected, is reportedly recovering well following his own treatment. But of course the treatment is most effective when the disease is caught early, so anyone in contact with rodents in the Western US is encouraged to be familiar with the bubonic plague’s symptoms: chills, general malaise, high fever (>39 °C/102.2 °F), and muscle cramps all typically occur before the characteristic bubo.
While surviving bubonic plague might make for some interesting cocktail chatter, it never hurts to play it safe, and maybe not feed the squirrels in the Pacific Northwest this year.








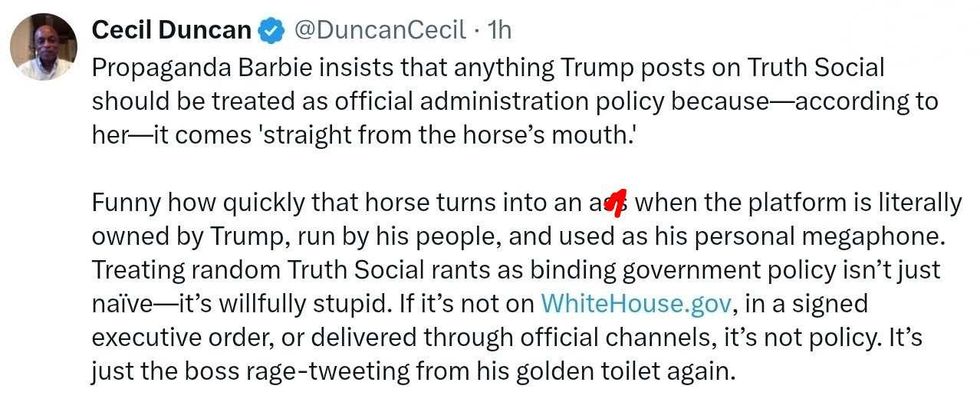 @DuncanCecil/X
@DuncanCecil/X @@realDonaldTrump/Truth Social
@@realDonaldTrump/Truth Social @89toothdoc/X
@89toothdoc/X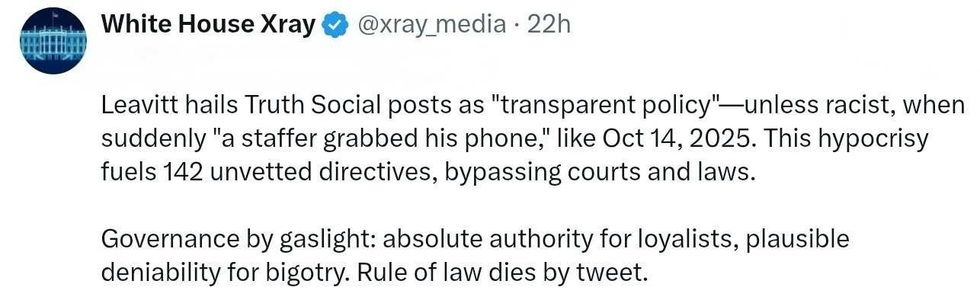 @xray_media/X
@xray_media/X @CHRISTI12512382/X
@CHRISTI12512382/X
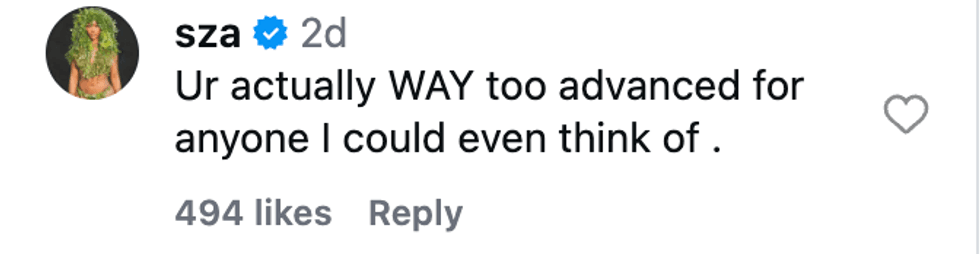 @sza/Instagram
@sza/Instagram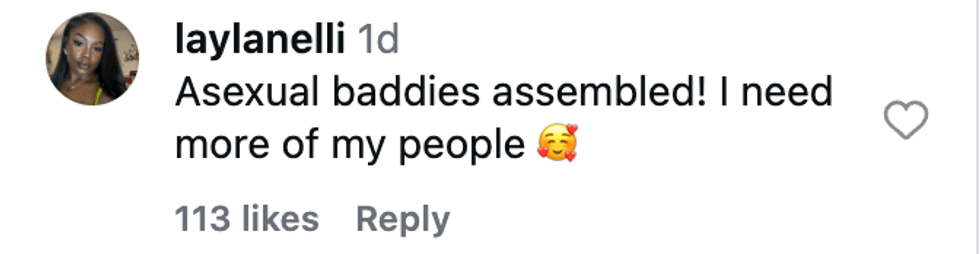 @laylanelli/Instagram
@laylanelli/Instagram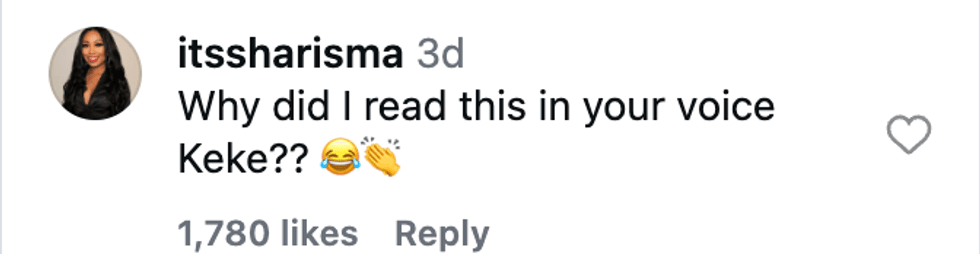 @itssharisma/Instagram
@itssharisma/Instagram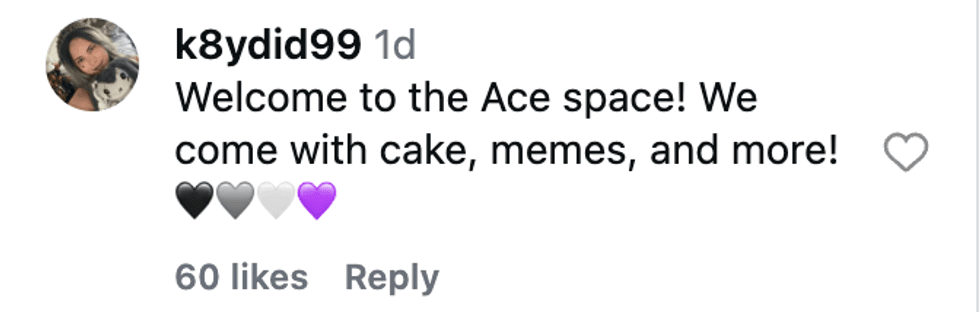 @k8ydid99/Instagram
@k8ydid99/Instagram @8thhousepath/Instagram
@8thhousepath/Instagram @solflwers/Instagram
@solflwers/Instagram @msrosemarienyc/Instagram
@msrosemarienyc/Instagram @afropuff1/Instagram
@afropuff1/Instagram @jamelahjaye/Instagram
@jamelahjaye/Instagram @razmatazmazzz/Instagram
@razmatazmazzz/Instagram @sinead_catherine_/Instagram
@sinead_catherine_/Instagram @popscxii/Instagram
@popscxii/Instagram